ADHD stands for attention-deficit/hyperactivity disorder. It’s a neurodevelopmental condition that affects both children and adults, influencing focus, impulse control, and activity levels. While many people associate ADHD with hyperactive kids, the reality is broader: ADHD can look different from person to person and can change over a lifetime. This article aims to explain what ADHD is, how it’s diagnosed, and practical ways to manage it in daily life.
What is ADHD? ADHD is not a character flaw or a sign of laziness. It’s a disorder rooted in brain development and functioning. People with ADHD often have differences in executive functions—skills that help with planning, organizing, sustaining attention, and regulating emotions. These differences can lead to challenges with schoolwork, work tasks, relationships, and daily routines. Importantly, ADHD exists on a spectrum. Some people have more pronounced inattention, others more hyperactivity and impulsivity, and many experience a mix of symptoms that ebb and flow across different settings.
Symptoms and how they present ADHD symptoms typically fall into three core areas:
- Inattention: difficulty sustaining focus, frequent careless mistakes, trouble following through on tasks, forgetfulness, distractibility, and trouble organizing activities.
- Hyperactivity: restlessness, fidgeting, difficulty staying seated, talking excessively, and an ongoing sense of being “on the go.”
- Impulsivity: acting without thinking, interrupting others, making decisions without considering consequences, and difficulty waiting for turns.
Children with ADHD may show more overt hyperactivity, while many adults present with primarily inattentive symptoms, such as racing thoughts, chronic disorganization, or forgetfulness. It’s also common to experience co-occurring conditions, such as anxiety, learning differences, or mood changes, which can complicate the picture.
Diagnosis: how ADHD is identified ADHD diagnosis involves a comprehensive evaluation by a qualified professional, such as a pediatrician, child psychologist, psychiatrist, or clinical social worker. The process typically includes:
- History and symptoms: gathering information about behavior across settings (home, school, work) and how long symptoms have persisted (often since childhood).
- Behavior checklists: standardized questionnaires completed by parents, teachers, or the individual.
- Medical assessment: ruling out other medical or environmental factors that could mimic ADHD symptoms.
- Information from multiple informants: teachers, parents, or partners provide different perspectives on behavior.
- Consideration of impairment: symptoms must interfere with functioning in daily life, not just be present.
ADHD is diagnosed when symptoms are persistent and cause impairment in two or more major settings (e.g., home and school/work) and were present before a certain age, according to established criteria. Because symptoms can overlap with other conditions, a careful differential diagnosis is essential.
Treatment: evidence-based options Effective ADHD management usually combines several approaches tailored to the individual. A well-rounded plan can include medication, behavioral therapies, skills coaching, and lifestyle adjustments.
- Medication
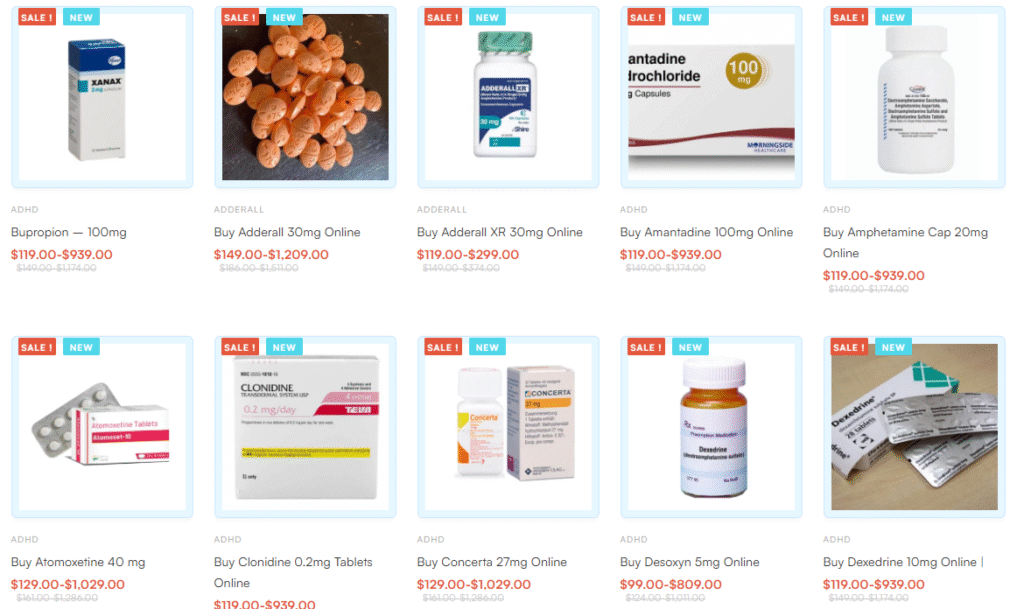
- Stimulants: The most common and well-studied medications for ADHD are stimulants (e.g., methylphenidate and amphetamine-based drugs). They can improve attention, executive function, and impulse control for many people.
- Non-stimulants: For those who don’t respond well to stimulants or experience side effects, non-stimulants (e.g., atomoxetine, guanfacine, clonidine) may be suitable.
- Important notes: Medication effectiveness and side effects vary. A healthcare professional should monitor treatment, adjust dosages, and assess benefits versus risks.
- Behavioral and psychotherapy approaches
- Cognitive-behavioral therapy (CBT): Helps with organization, problem-solving, time management, and emotional regulation.
- ADHD coaching: Focused support to set goals, build routines, and sustain accountability.
- Family or parental training: Strategies to create structure and reduce conflict at home.
- Skills and environmental supports
- Structure and routines: Predictable schedules, clearly defined tasks, and consistent expectations can reduce overwhelm.
- External aids: Planners, reminder apps, timers, checklists, and color-coding systems help with organization and follow-through.
- Workplace accommodations: Flexible schedules, quiet workspaces, written instructions, and task segmentation can improve productivity.
- Lifestyle and wellness
- Sleep: Regular, sufficient sleep improves attention and mood.
- Exercise: Regular physical activity supports executive function and reduces restlessness.
- Nutrition: Balanced meals and mindful snacking can stabilize energy and concentration.
- Mindfulness and stress management: Techniques like deep breathing or short meditations can help with impulse control and emotional regulation.
Daily management tips
- Use a trusted system: Choose a planning method (digital calendar, paper planner, or a hybrid) and stick to it.
- Break tasks into chunks: Large projects feel overwhelming; break them into smaller, actionable steps with deadlines.
- Time management: Set timers (e.g., 25-minute work blocks with short breaks) to sustain focus.
- Reduce clutter: A tidy workspace minimizes distractions. Keep only what you need for the task at hand.
- Minimize interruptions: Create boundaries for notifications or set dedicated focus periods.
- Build routines: Consistent morning and evening routines help reduce decision fatigue and improve overall control.
ADHD in school and work
- In schools: Diagnosis can lead to accommodations such as extended time on tests, preferred seating, or note-taking support. A 504 plan or an individualized education plan (IEP) may be appropriate, depending on the region and the individual’s needs.
- In the workplace: Employers can offer accommodations like flexible scheduling, clear written instructions, task lists, and a quiet workspace. Time management tools and coaching can also be valuable.
Common myths and misconceptions
- ADHD is not a result of laziness or discipline problems. It’s a neurodevelopmental condition with real brain-based differences.
- ADHD does not automatically disappear with age. Some people continue to experience symptoms into adulthood, though presentation may change.
- Children with ADHD do not outgrow it by themselves; many benefit from early intervention and ongoing supports.
When to seek help If you notice persistent inattention, hyperactivity, or impulsivity that interferes with daily life for you or your child, consider speaking with a healthcare professional. A formal assessment can determine whether ADHD is present and guide an appropriate treatment plan. Early intervention often improves long-term outcomes.
Building a supportive path Living with ADHD is about finding the combination of strategies that fits your life. Some people thrive with medication and therapy; others focus on coaching and environmental changes. The key is to approach ADHD with patience, a willingness to try different tools, and support from family, teachers, or colleagues.
Final thoughts ADHD is a real, manageable condition that can be addressed with a thoughtful mix of medical, psychological, and practical strategies. By understanding symptoms, seeking a proper diagnosis, and applying evidence-based treatments and daily routines, individuals with ADHD can achieve focus, structure, and success in school, work, and everyday activities.
Note: This article is for general educational purposes and does not constitute medical advice. If you’re concerned about ADHD symptoms for you or a loved one, please consult a qualified healthcare professional for an evaluation and personalized guidance.